Prior Authorization

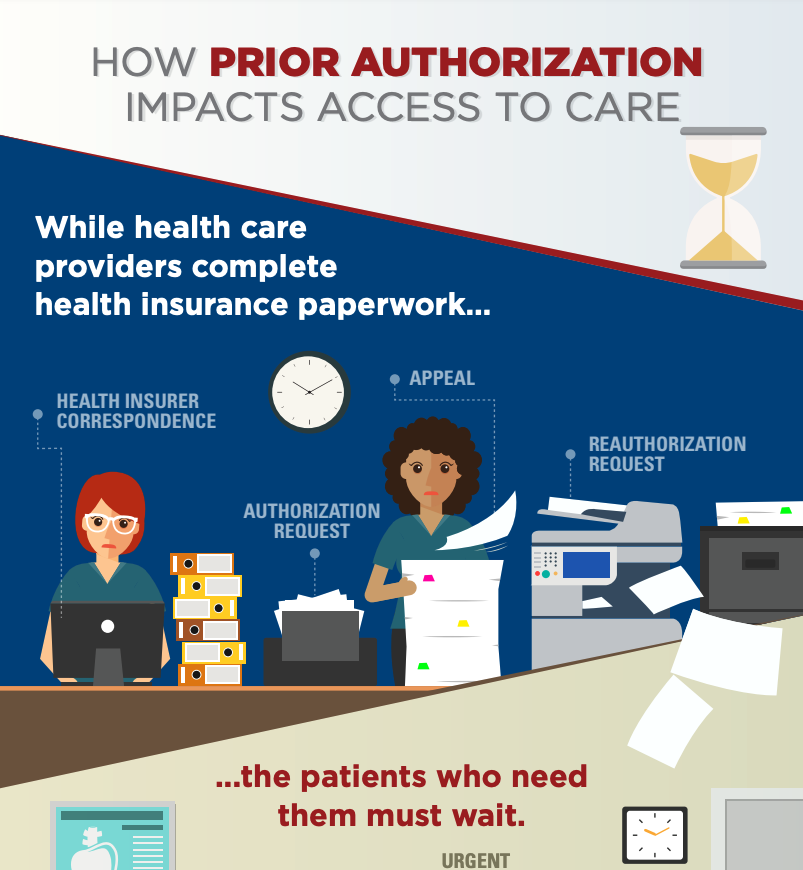
Prior authorization is a tactic in which pharmacy benefit managers and health insurers require a clinician to get approval before providing a service or filling a prescription, often/unnecessarily delaying care.
Seniors’ Act
The Improving Seniors’ Timely Access to Care Act, or Seniors’ Act, would provide patient and provider transparency and streamline the prior authorization process under Medicare Advantage.
PCSK9 Rejections
PCSK9 inhibitors help lower “bad” cholesterol. But access has remained a major hurdle, especially for at-risk populations. In recent years, Medicare has rejected more than half of patients for PCSK9 inhibitors.
Prior Authorization Resources
Graphics
Prior Authorizations stand Between Patients and Treatment
Social media graphic
Videos
Barriers to Patient Access: Step Therapy
When prior authorization delays treatment, patients can see their symptoms worsen and their relationship with their physician erode.
Jeff - Familial Hypercholesterolemia (FH) Story
Jeff’s story explains why it’s so important to support medical innovation – and access to new medicines that result from that innovation.
The Prior Authorization Battle
Hear from heart patients and health care providers about the burden of prior authorization.
Lynne Braun, CNP, PhD, Discusses Cardio Health
Lynne Braun, CNP, PhD, discusses the impact of health insurers' prior authorization on cardiovascular patients.
Seth Baum, MD, Discusses Cardio Health
In this video, Seth Baum, MD, explains how every one of his patients was denied access to a PCSK9 inhibitor.